Abstract
Pediatric acute myeloid leukemia (AML) is the deadliest malignancy in children. Despite maximally intensive therapy, inclusive of chemotherapy and hematopoietic stem cell transplant, approximately 20% of patients experience recurrent disease. These patients are also burdened with treatment-related toxicities. Significant improvements in survival in pediatric AML patients necessitate the incorporation of rational targeted therapies with reduced toxicity. Recent studies demonstrate that PRMT5 knockout or inhibition in syngeneic mouse models of KMT2A (MLL) rearranged leukemic cells increased disease latency (Serio et al., Oncogene, 37:450, 2018; Kaushik et al., Leukemia, 32:499, 2018), indicating that PRMT5 is a potential therapeutic target in pediatric AML. However, there are no reports testing the efficacy of PRMT5 in PDX models of pediatric AML.
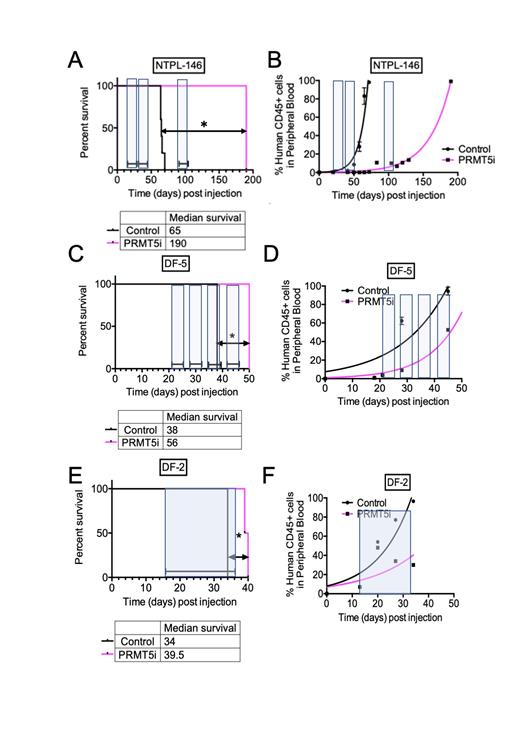
We evaluated the preclinical efficacy of C220, a potent and selective PRMT5 inhibitor (PRMT5i) (Pastore et al., Cancer Discovery, 10:1742, 2020) in three distinct patient-derived xenograft (PDX) models of KMT2A rearranged AML. Based on the model used for the study, 3-5 million AML cells were injected intravenously in NSG-B2m mice. Disease progression was monitored by evaluating the percentage of human cells in mouse peripheral blood at periodic intervals by flow cytometry. At 2-3 weeks post transplantation, when human cells were detectable in peripheral blood, mice were randomly assigned to control (n=4-5) or treatment (n=2) groups. C220 was administered daily p.o. at a dose of 15 mg/kg for seven days with a break of two days. Mice were dosed with 2-3 additional cycles (indicated in the figure by shaded areas) based on their health status. Mice were monitored daily for experimental endpoints that included body condition score and human cell percentages in peripheral blood. Kaplan-Meier survival plots were generated based on the time when mice were euthanized because they met experimental endpoints.
Chronic dosing of C220 prolonged survival and delayed the rise in percentage of human AML cells in mouse peripheral blood in all 3 PDX models (Fig. 1B, D, F). In the NTPL-146 model (KMT2A-MLLT1 fusion), a 135-day improvement in median survival was observed with C220-treatment (Fig. 1A). In the DF-2 (KMT2A-MLLT10 fusion) and DF-5 (KMT2A-MLLT4 fusion) models, which showed a faster engraftment compared to NTPL-146, there was a 5.5-day and 18-day improvement in median survival respectively (Fig. 1C, E). The improvement in median survival was statistically significant in all models (*P<0.05). In conclusion, C220 was effective in controlling leukemia progression and improving survival in KMT2A rearranged PDX models of pediatric AML.
Gopalakrishnapillai: Geron: Research Funding. Zhang: Prelude Therapeutics: Current Employment. Ruggeri: Prelude Therapeutics: Current Employment, Current equity holder in publicly-traded company. Scherle: Prelude Therapeutics: Current Employment, Current equity holder in publicly-traded company. Barwe: Prelude Therapeutics: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal